| host_defenses.pptx | |
| File Size: | 16394 kb |
| File Type: | pptx |
HOST DEFENSES
It is easy for us to take for granted, waking up in the morning, taking a full, deep breath and feeling healthy. But like all good things, you never know what you got... until it's gone!
Most of us have experienced feeling pretty lousy from time to time. Some of us may have been unlucky enough to have been so ill that we may have had to be hospitalized or may have been in a life-threatening situation due to an infectious disease.
The human body and the pathogens that can infect them, have co-evolved since the beginning of human history. Over time, adaptations evolved, not only on the part of the pathogen (discussed on the pathogenicity page), but on the part of the human body as well.
The human body has developed specialized structures and mechanisms to pathogens.
The human body has developed specialized structures and mechanisms to pathogens.
The body's first line of defense is the "innate nonspecific immune system".
- the acquired specific immune system.
The body has three strategies for defending against disease.
- THE FIRST LINE OF DEFENSE - Prevention - Keep the pathogen from invading the body. This is the first line of defense and is accomplished by the body's chemical and physical surface barriers.
- THE SECOND LINE OF DEFENSE - Attack - Attack the pathogen and defend the body's cells and tissues from infection. This is the second line of defense. These defenses are the internal cellular and chemical defenses of the body that kick into action if the pathogen enters the body.
- THE THIRD OF DEFENSE - Destroy - Destroy the invading pathogen. This is the third line of defense and it is accomplished as the immune response.
The first and second lines of defense are considered "nonspecific mechanisms of defense", because they are defenses of the body that generally prevent any microorganism from invading the body. The first and second lines of defense are "innate", meaning that these are defenses that we are born with.
In contrast, the third line of defense is acquired, adaptive and specific!. We acquire adaptive immunity by being exposed to different substances, chemicals, or organisms throughout our lifetime, but especially in our early childhood. These "foreign" substances become training for the immune system to learn what belongs to the body and what does not belong.
In contrast, the third line of defense is acquired, adaptive and specific!. We acquire adaptive immunity by being exposed to different substances, chemicals, or organisms throughout our lifetime, but especially in our early childhood. These "foreign" substances become training for the immune system to learn what belongs to the body and what does not belong.
The First Line of Defense
- The Innate Nonspecific Physical and Chemical Barriers
|
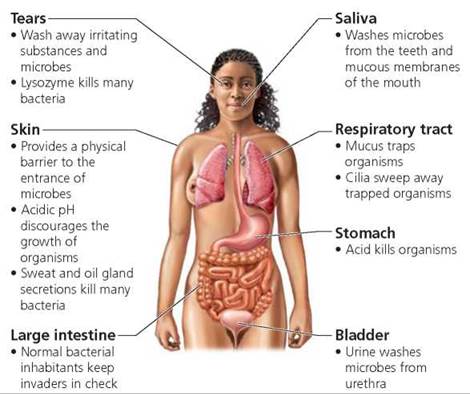
The First Line of Defense are the physical and chemical barriers that line the parts of your body that are exposed to the outside world, that are specially suited to prevent microbes from freely entering the body.
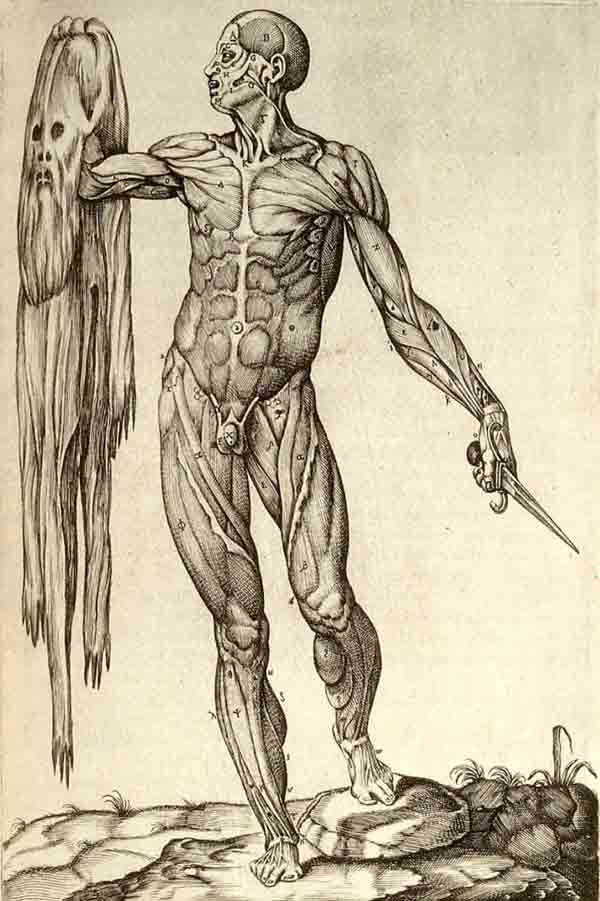
Physical barriers of the first line of defense:
Your skin is an organ. In fact, your skin is, by far, the largest organ of your body. Your precious skin wraps your delicate inner tissue in a protective blanket and shields you from the elements of the environment, and prevents microbes from easily passing into your body. One of the ways that the epithelial cells that make up your skin form this preventative barrier is through the formation of cell junctions.
|
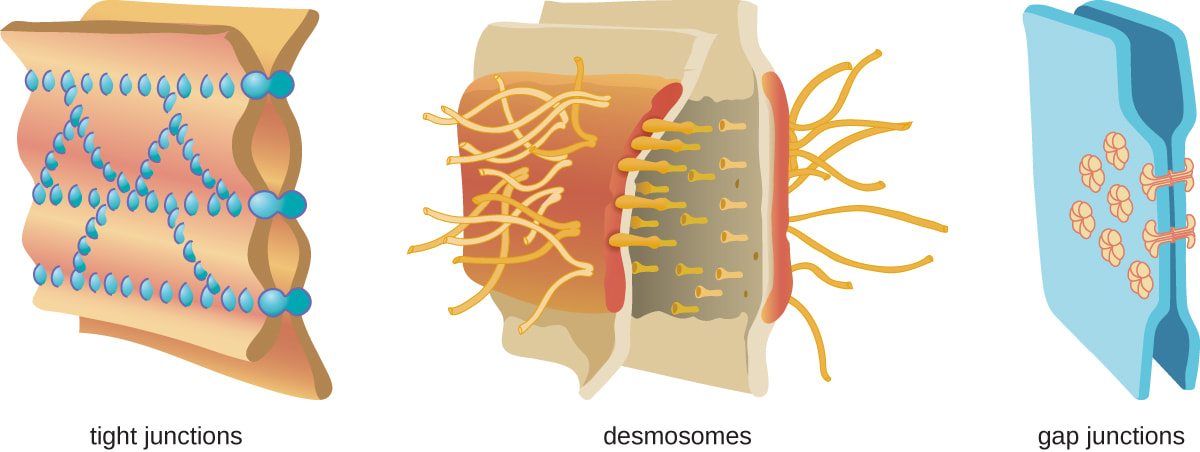
cell junctions
Cell junctions such as tight junctions, desmosomes, and gap junctions, help to prevent pathogens from easily passing into the body.
Tight junctions allow the membranes of adjacent cells to come into physical contact with one another, to prevent, limit, or control the movement of substances (or microbes) between cells. Desmosomes create a barrier between cells by using intermediate fibers that string adjacent cells together. Gap junctions are cytoplasmic bridges that connect adjacent cells and allow for cell to cell communication or chemical signaling. This configuration does not leave much room between adjacent cells for microbes to pass. (illustration credit: modification of work by Mariana Ruiz Villareal)
CELL JUNCTIONS
|
mucous membranes
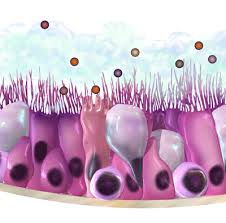
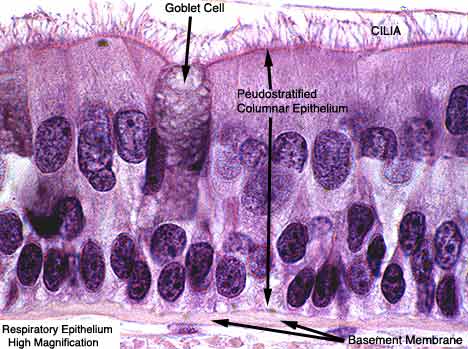
Mucous membranes are found in the nose, mouth, lungs, and urinary and digestive tracts. These membranes are made up of goblet cells and ciliated epithelial cells.
The goblet cells secrete a moist, sticky substance called mucus. Mucus covers and protects delicate cell layers while trapping microbes and other small particles that come into contact with it. Mucus also contains some antimicrobial peptides. Mucous membranes are lined with ciliated epithelial cells which function to sweep away pathogens caught in the mucus. The Mucus is expelled from the body through coughing up or swallowing the pathogen and the mucus it is trapped in. |
|
|
Chemical barriers of the first line of defense:
The first line of defense also involves some chemical defenses as well. For example. the skin has sweat glands that secrete sweat and sebaceous glands that secrete oil. Sweat is acidic which can discourage microbial growth and oily secretions also have some antimicrobial qualities. The acidic environments of urinary tract, stomach and vagina discourages microbial growth. stomach and vagina. Saliva and tears contains an enzyme called lysozyme that functions to block the synthesis of the bacterial cell wall. When the bacterial cell wall cannot be synthesized or repaired, the bacteria dies soon after.
|
The Second Line of Defense
- The Innate Nonspecific Internal Cellular and Chemical Defenses

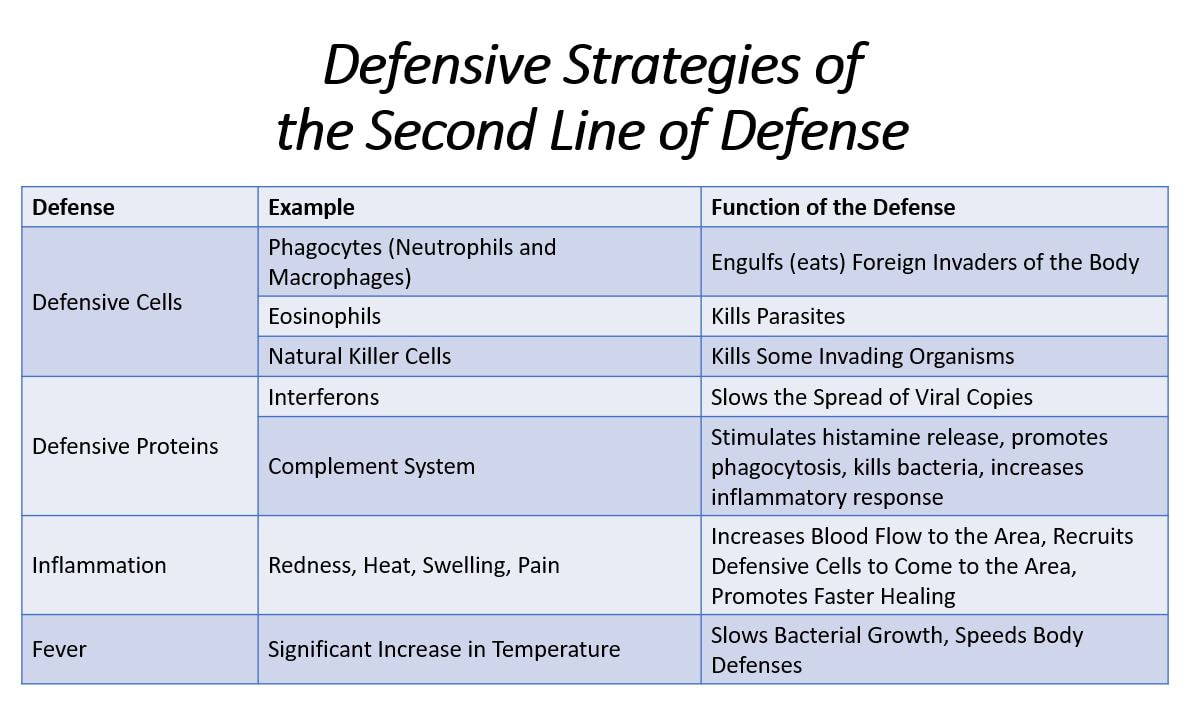
Second Line of Innate Defense: Occasionally, a pathogenic organism will penetrate a person's first line of defense and invade the body. When this breach occurs, the body launches the second line of defense. The second line of defense involves the activation of specialized "defensive cells" and the mobilization of proteins. The processes leads to inflammation and fever. Interestingly, the inflammation and fever is actually not being caused directly by the pathogen, but is being caused as the defensive mechanisms of your body in response to the presence of the pathogen.
Defensive Cells
|
Defensive cells. are white blood cells called phagocytes that "eat" unwanted invaders of the body, as well as dead or damaged cells. The term phagocytes comes from the words for "phage" which means "to eat", and "cyte" which means "cell". So phagocytes will "eat" unwanted entities found in the body by engulfing them and chemically breaking them down in a process called phagocytosis. Phagocytes are nonspecific and will get rid of pathogenic organisms, as well as dead or damaged cells or unwanted debris found in the body. In a sense, they are the body's janitorial service.
|
|
The human body has two types of white blood cells that are phagocytes; the neutrophils and the monocytes. Both of these are types of white blood cells, but they have unique morphology, physiology and different mechanisms of action.
neutrophils
The neutrophils are one of the two types of white blood cells categorized as phagocytes.. They are the first type white blood cell to respond to a foreign invader or unwanted particle in the body. You can think of the neutrophiles as the "first responders" of the body's emergency response team. When the neutrophils arrive at the scene, they immediately respond by consuming the unwanted entity.
monocytes
|
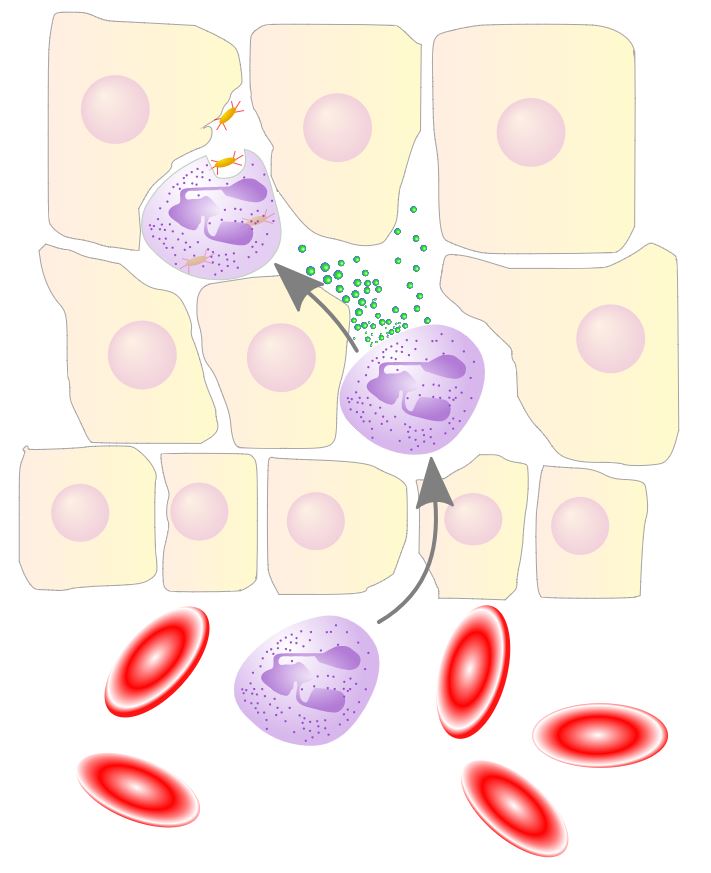
Monocytes (macrophages) are the other types of white blood cells that are categorized as phagocytes. The monocytes are delivered to the lymphatic fluids of the body through the circulatory system. Once the monocytes have reached the desired destination, they leave the blood vessels of the circulatory system and enter the fluid of the body where they mature (or differentiate) into macrophages. Macrophages are able to consume large particles of debris and large amounts of unidentified organisms that the macrophages have determined do not belong in the body. Macrophages are less picky eaters than neutrophils. The macrophages are able to consume a wider variety of substances, they can consume larger individual particles or entities and can consume higher quantities than neutrophils.
eosinophils
|
|
Some pathogens are too large to be consumed even by macrophages. In these cases, our body's utilize another type of white blood cell called the eosinophils. The eosinophils specialize in attacking pathogens that are too large for the macrophages to engulf, such as parasitic worms. Eosinophils function by positioning themselves close to the pathogen and releasing enzymes that kill the organism and break it down into smaller pieces. At this point, the macrophages can remove the smaller pieces using phagocytosis.
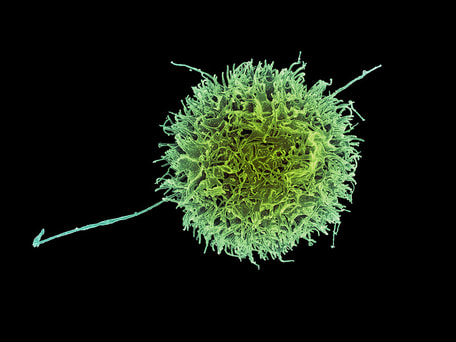
natural killer cells
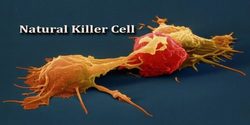
Natural killer cells are white blood cells that are constantly on patrol seeking out any suspicious characters it finds in the body. Natural killer cells (NK cells) will indiscriminately kill anything that it perceives as "abnormal". This means that the NK cells will not only destroy foreign invaders, but will also destroy the body's own cells that may show signs of mutation, or infection or disease. For example, host cells that have become cancerous or that have become infected with a virus are likely targets for the NK cells. The natural killer cells destroy their target by coming into direct contact with the suspicious cell and secreting proteins that degrade the structural integrity of its membrane until the cell dies.
Defensive Proteins
The second line of defense also includes the action of defensive proteins, such as interferons and the proteins of the complement system.
interferons

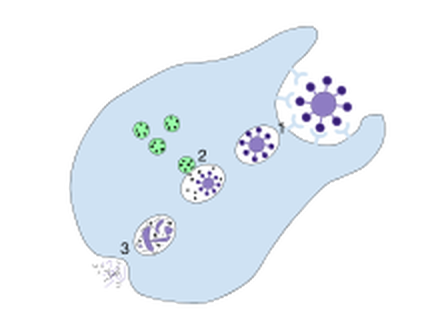
Interferons are proteins which act to slow down the process of viral reproduction. Once a cell has become infected with a virus, its days are numbered. Cells infected with a virus will secrete small proteins called interferons that will interfere (hence the name) with the ability of the virus to spread to nearby cells.
Interferons accomplish their viral "interference" with a one-two punch, that comes in two distinct phases. The first phase, is to recruit macrophages and natural killer (NK) cells to destroy and eliminate cells that have already become infected. The second phase involves defending the remaining healthy uninfected cells from invasion. The interferon protein protects these cells by stimulating those cells to produce additional proteins that act to inhibit viral replication should infection occur. This is very effective, because the virus cannot reproduce without the hostile takeover of a host cell. Without a host cell, the virus cannot reproduce and the virus stops spreading. This allows the white blood cells to gain the upper hand and win the battle.
Interferons accomplish their viral "interference" with a one-two punch, that comes in two distinct phases. The first phase, is to recruit macrophages and natural killer (NK) cells to destroy and eliminate cells that have already become infected. The second phase involves defending the remaining healthy uninfected cells from invasion. The interferon protein protects these cells by stimulating those cells to produce additional proteins that act to inhibit viral replication should infection occur. This is very effective, because the virus cannot reproduce without the hostile takeover of a host cell. Without a host cell, the virus cannot reproduce and the virus stops spreading. This allows the white blood cells to gain the upper hand and win the battle.
Pharmaceutical preparations of interferon have been shown to be effective against certain cancers and viral infections including hairy cell leukemia, Kaposi's sarcoma, hepatitis C, HPV, and herpes..
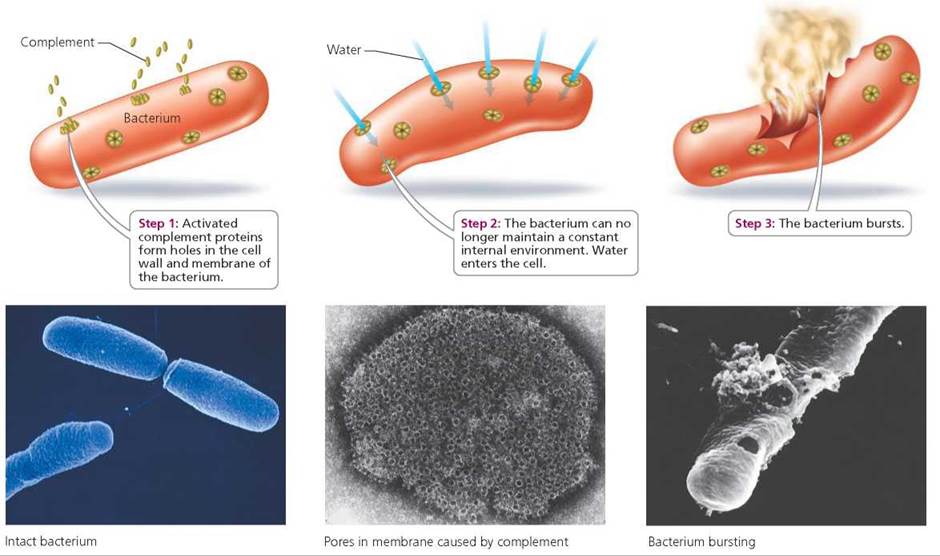
the complement system
The complement system refers to a large group of proteins that work to "complement" or enhance the effects of body's other defense mechanisms. These proteins are always present in the circulatory system of the body, but only become activated when an infection is sensed. The functions of the activated complement system includes the following:
- Destroying the pathogen. Pokes holes in a pathogen's membrane, which leads to cell bursting.
- Enhancing phagocytosis. Complement enhances phagocytosis by recruiting macrophages and neutrophils to the site of infection and by creating a handle on the membrane of the pathogen so it becomes easier to grip.
- Stimulating the inflammatory response. Complement causes blood vessels to widen which promotes blood flow to the area and increased access for white blood cells.
Inflammation |
|
|
Inflammation occurs as the result of some sort of internal injury or damage to the tissues. Most of us have experienced inflammation at some point our lives. You may recall that the experience is not very pleasant. In fact, the inflammatory response is characterised by four signs:
|
Redness.
- Damaged cells release chemical signals including histamines at the site of the injury. The histamines effectively dilate or widen the blood vessels in the area, promoting additional blood. flow and making the area appear red from the outside of the body. The increased blood flow to the injured area allows defensive cells and proteins to gain access to the area more easily.
- Increased blood flow also elevates the temperature in the area of injury. The increased temperature also increases the metabolic rate of the host cells in the region which promotes healing.
- The histamines in the area cause the small blood vessels (the capillaries) to become more permeable. This allows more fluids and substances to pass from the the bloodstream to the tissues, which causes swelling. However, the swelling brings in vital nutrients and liquids from the blood stream that promote healing.
- Pain often accompanies inflammation due to excessive fluid that may have pressed on nerves, Pain can also be experienced due to toxins released by bacterial or by prostaglandins. Pain is unpleasant, but it is protective. It is your body's way of letting you know something is wrong and needs attention. Pain also causes a person to protect the area from additional injury.
Inflammation paves the way for defensive cells to gain access to the area of injury by widening the blood vessels and increasing capillary permeability. This allows phagocytes to swarm as the first responders that come calling as soon as the chemical message released by damaged cells is received. In a matter of only minutes, the neutrophils arrive on the scene by squeezing their way through the capillary walls and commence engulfing unwanted organisms and debris. Macrophages arrive soon after to assist in gobbling up unwanted organisms and particles. At times the area can become filled with dead cells, dead microbes and phagocytes that take on the form of puss that can leak or ooze out of a wound.
Fever
The Third Line of Defense
- Adaptive Immune Response
The first and second lines of defense are nonspecific so they are ready to go at a moment's notice. This is kind of like the fast food drive through. You don't get a custom made order, but it is a one size fits most and most if the time it's good enough to feed your hunger. However, sometimes you really need something special that is prepared in a unique way, to meet your specific needs. Well, that will take a little time, but it will be customized and it will be "just what the doctor ordered!"
Sometimes the one size fits most approaches of the first and second lines of defense aren't enough to eradicate the pathogen making the person ill. It is time for that special order, the third line of defense!! The third line of defense refers to the specific responses and memory of the immune system.
lymphocytes
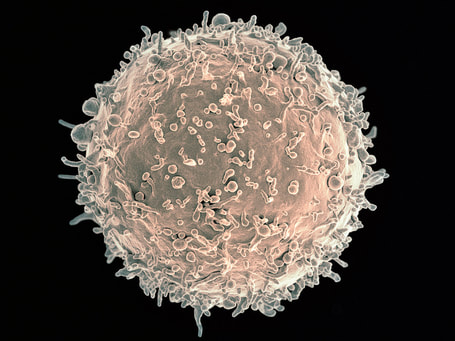
Lymphocytes are the white blood cells that are responsible for both the specificity and the memory of the adaptive immune response.
There are two types of lymphocytes:
- The B cells
- The T cells
mode from haematopoietic stem cells in the bone marrow, but they develop in different organs of the body. The B cells continue to develop in the bone marrow, while the T cells, travel to the thymus gland to develop.
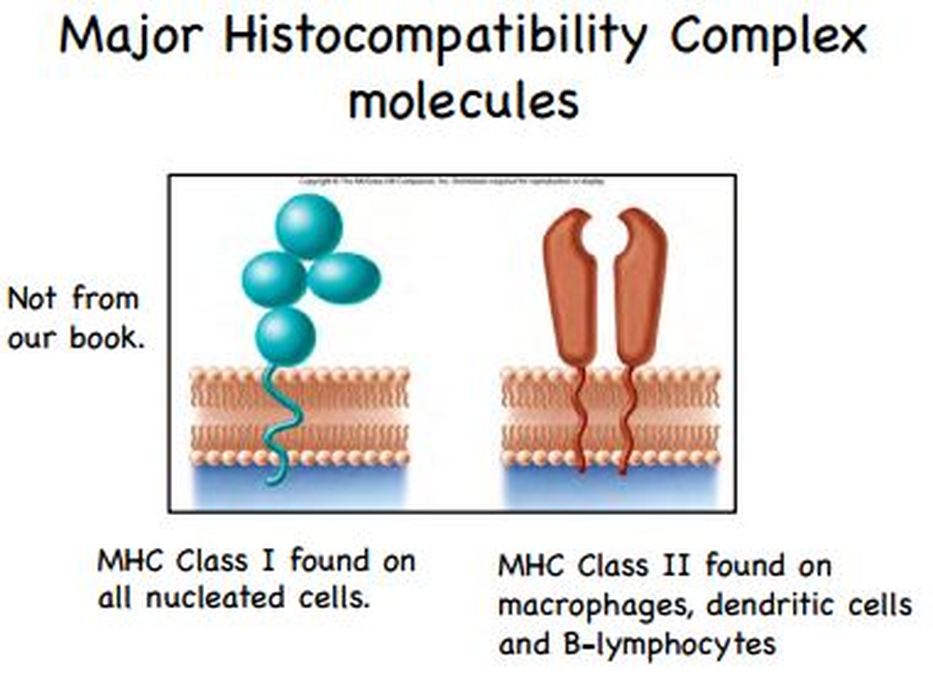
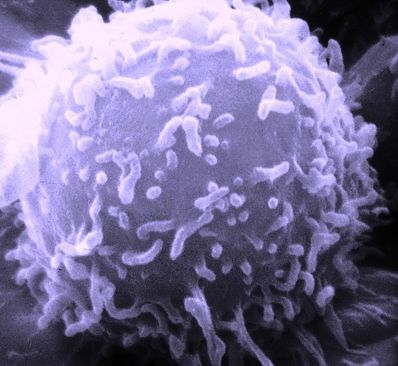
The T cells specialize in learning how to distinguish between the cells that do belong in the body and the ones that do not belong in the body by screening their major histocompatibility complexes (MHCs). Once the T cells are fully mature (differentiated) they leave the thymus and circulate through the body on a permanent mission of "seek and destroy".
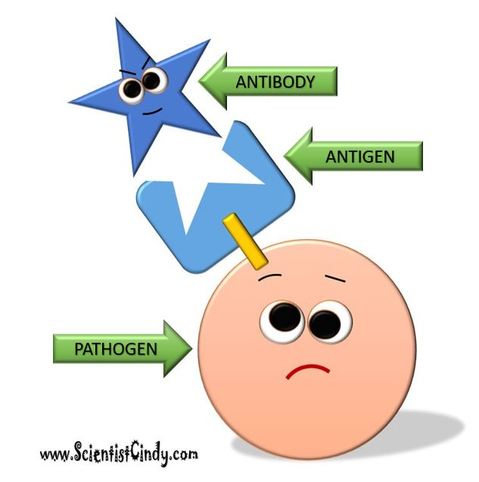
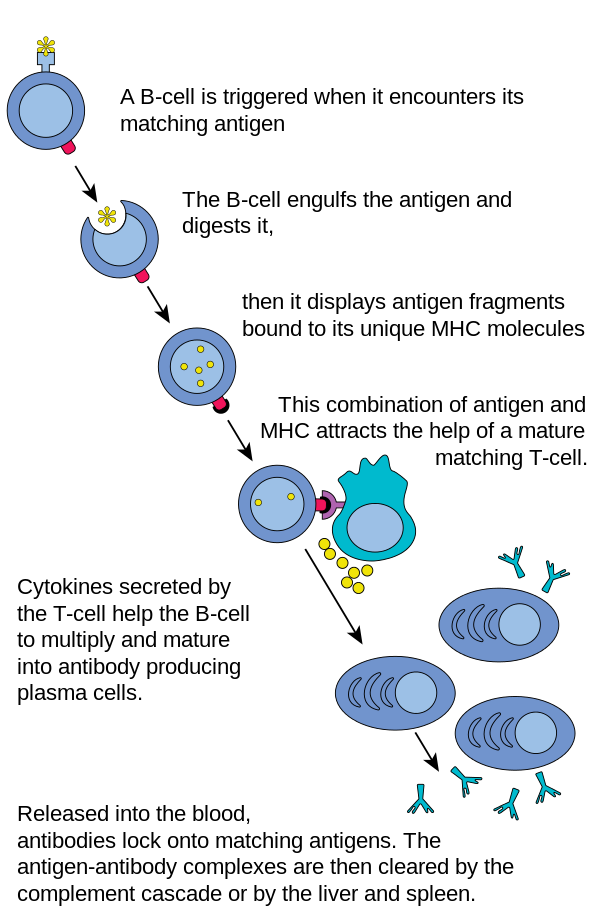
When an antigen is detected, B cells and T cells will be recruited that have receptors bearing the correct configuration to bind to the invader in a lock and key manner so that it can be destroyed.
The T cells specialize in learning how to distinguish between the cells that do belong in the body and the ones that do not belong in the body by screening their major histocompatibility complexes (MHCs). Once the T cells are fully mature (differentiated) they leave the thymus and circulate through the body on a permanent mission of "seek and destroy".
When an antigen is detected, B cells and T cells will be recruited that have receptors bearing the correct configuration to bind to the invader in a lock and key manner so that it can be destroyed.
Step One: Identifying "Self" from "Nonself"
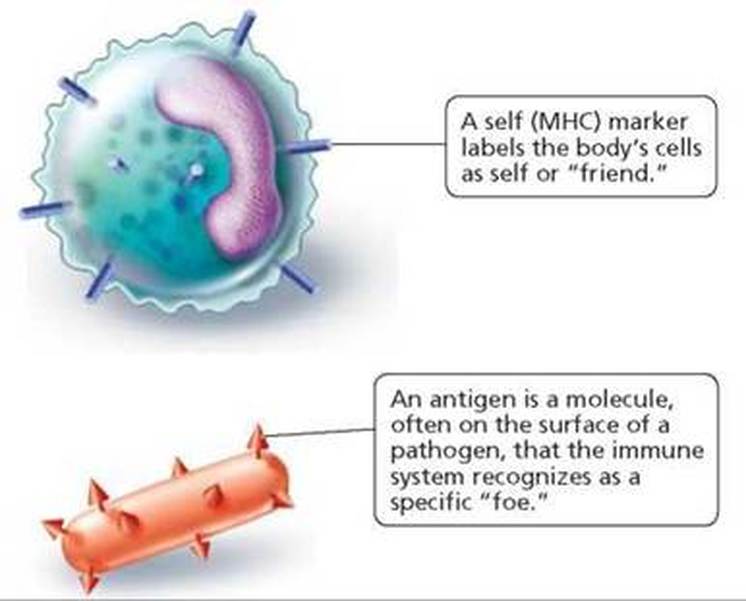
` The cells of each person's body has a unique molecular marker that tells the cells of their immune system, that that cell is part of the body... that the cell belongs there and is a friend and should not be destroyed. These molecular markers are called Major Histocompatibility Complexes. (MHC). Only identical twins would have identical MHCs.
White blood cells travel around the body searching for foreign invaders. MHCs (under normal circumstances) will not elicit an immune response. When white blood cells encounter a foreign cell, they search the cell's surface attempting to recoignize an MHC. Instead of finding the familiar MHC, the white blood cells finds an a different molecular marker on the cell's surface generically called an "antigen". An antigen is any molecule capable of inducing an immune response.
Lymphocytic B-Cells
Lymphocytic B cells receptors that detect specific antigens. When the B cell is mature, it leaves the bone marrow and resides in the lymph of the body or the lymphatic organs. When the B cell encounters its antigen, its receptor with the specialized antibodies binds to it and does not let go. The lymphocytic B cell engulfs the bound cell through the process of endocytosis.
Once the unwanted cell has been engulfed, the B cell will then display the antigen from the target cell on its own surface, as a MHC-II molecule. This is called an MHC-II to distinguish it from the MHC (or more specifically MHC-I).
Once the unwanted cell has been engulfed, the B cell will then display the antigen from the target cell on its own surface, as a MHC-II molecule. This is called an MHC-II to distinguish it from the MHC (or more specifically MHC-I).
Lymphocytic T Cells
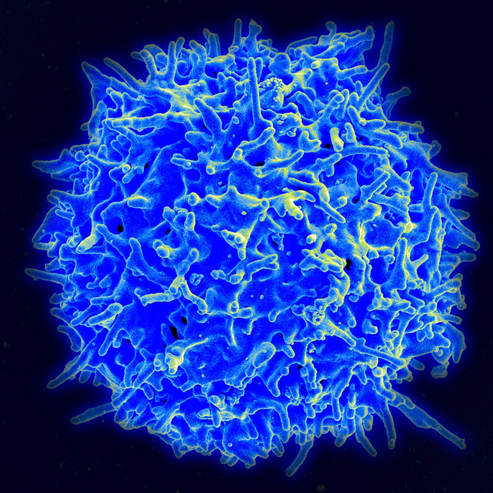
The T cell will then bind to the MHC-II complex and become activated. The activated T cell releases cytokines that causes the B cells to undergo rapid cell division. This results in thousands of new B cells; some of which become memory cells. Memory cells will retain the antigen information from the infection that lead to their creation. In the event that the body becomes infected with the same (or very similar) pathogen in the future, the memory cells will respond by dividing and differentiating into plasma cells. As plasma cells, they release vast numbers of antibodies that will flow through the circulatory system.