BLOOD LAB
LAB EXERCISE: Blood Cell Counts, Hemoglobin, Hematocrit, Blood Typing
Summary
Blood tests are laboratory analyses performed on blood samples, usually from a vein in the arm. Blood tests can provide useful information about a persons’ health.
Two sets of blood tests are routinely used in the hospital setting:
1) comprehensive metabolic panel
2) complete blood count
A comprehensive metabolic panel (CMP) is a blood chemistry profile that provides a quick check for a wide variety of problems, such as high glucose, electrolyte imbalances, and markers of kidney or liver problems.
A complete blood count (CBC) is a blood panel that provides information about the patient’s blood, such as the cell count for each cell type and the concentration of various proteins and minerals. CBC tests are a valuable tool for a variety of disorders such as anemia, infection, and blood diseases.
Summary
Blood tests are laboratory analyses performed on blood samples, usually from a vein in the arm. Blood tests can provide useful information about a persons’ health.
Two sets of blood tests are routinely used in the hospital setting:
1) comprehensive metabolic panel
2) complete blood count
A comprehensive metabolic panel (CMP) is a blood chemistry profile that provides a quick check for a wide variety of problems, such as high glucose, electrolyte imbalances, and markers of kidney or liver problems.
A complete blood count (CBC) is a blood panel that provides information about the patient’s blood, such as the cell count for each cell type and the concentration of various proteins and minerals. CBC tests are a valuable tool for a variety of disorders such as anemia, infection, and blood diseases.
Precautions: ***Students must work with their own blood only. If you have a medical condition that prevents you from participating, please tell your instructor for accommodations.
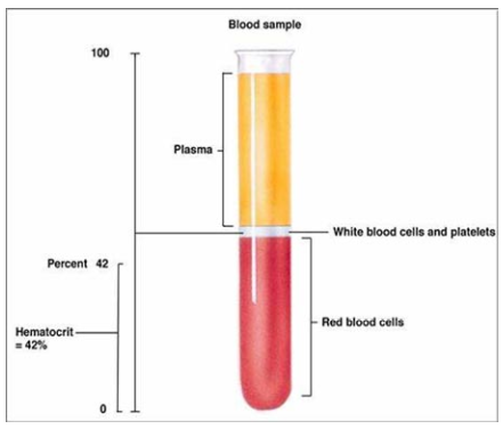
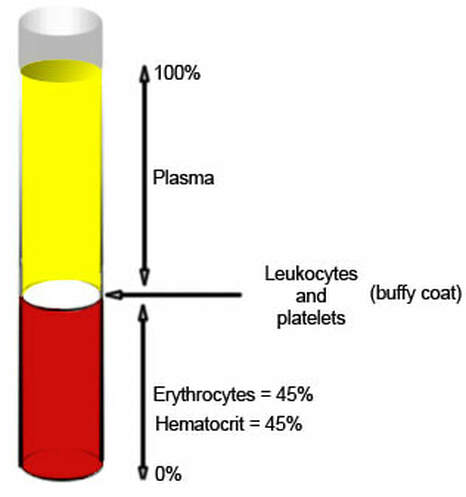
Blood is composed of plasma (composed of mainly water, proteins, & electrolytes) and formed elements (cells). The cells that circulate in the blood include leukocytes (white blood cells), erythrocytes (red blood cells), and thrombocytes (platelets). Abnormally high or low blood cell counts may indicate a variety of diseases and is the main reason why CBCs are routinely performed.
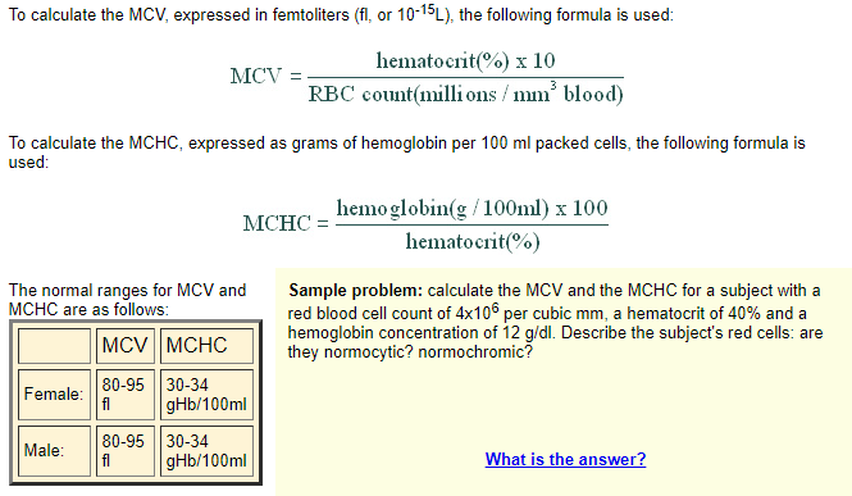
Blood cells counts can be counted manually using a hemocytometer. A hematocrit provides the fraction, or percent, of red blood cells in the blood. The amount of hemoglobin in blood (expressed in g/dL) can be measured with a hemoglobinometer; a low level of hemoglobin can be a sign of anemia. Mean corpuscular hemoglobin concentration (MCHC), is the average amount of hemoglobin in red blood cells and can be calculated using hemoglobinometer and hematocrit results. Mean corpuscular volume (MCV) is the average volume of red blood cells.
Red blood cell count (106 RBCs/μL/mm3) (RBCs/μL/ mm3)
Hemoglobin concentration of blood (g/dL)
Hematocrit (% RBCs)
Mean corpuscular hemoglobin (MCH) (μg/cell)
Mean corpuscular hemoglobin concentration (MCHC) (%) = ([hemoglobin] * 100%) / hematocrit • Mean corpuscular volume (MCV) (um3) =(Hematocrit * 10) / (RBC count)
Hemoglobin concentration of blood (g/dL)
Hematocrit (% RBCs)
Mean corpuscular hemoglobin (MCH) (μg/cell)
Mean corpuscular hemoglobin concentration (MCHC) (%) = ([hemoglobin] * 100%) / hematocrit • Mean corpuscular volume (MCV) (um3) =(Hematocrit * 10) / (RBC count)
LAB EXERCISE A. Hemoglobin Concentration
What is hemoglobin?Hemoglobin is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues back to the lungs.
Hemoglobin is made up of four protein molecules (globulin chains) that are connected together; two alpha-globulin chains and two beta-globulin chains. Each globulin chain contains an important iron-containing porphyrin compound called heme. Embedded within the heme compound is an iron atom that is vital in transporting oxygen and carbon dioxide in our blood. The iron contained in hemoglobin is also responsible for the red color of blood.
Hemoglobin is made up of four protein molecules (globulin chains) that are connected together; two alpha-globulin chains and two beta-globulin chains. Each globulin chain contains an important iron-containing porphyrin compound called heme. Embedded within the heme compound is an iron atom that is vital in transporting oxygen and carbon dioxide in our blood. The iron contained in hemoglobin is also responsible for the red color of blood.
|
Equipment • Placemat • Hemoglobinometer • Test strips • Lancet • Alcohol swab • Band Aid
Protocol:
|
A common method for measuring the hemoglobin content of blood makes use of an instrument known as a hemoglobinometer, which compares the colour of light passing through a hemolyzed blood sample with a standard colour. The results of the test are expressed as grams of hemoglobin per 100 ml of blood.
How to Use a Hemoglobinometer
A hemoglobinometer is an instrument used to determine the hemoglobin content of the blood by spectrophotometric measurement. Portable hemoglobinometers provide easy and convenient measurement, which is particularly useful in areas where no clinical laboratories are available.
|
Normal hemoglobin concentration varies for males and females:
o Males: 13 – 18 g/dL
o Females: 12 – 16 g/dL
● Calculate your Mean Corpuscular Hemoglobin Concentration.
o Mean corpuscular hemoglobin concentration (MCHC) in (%) = ( [hemoglobin] * 100% ) / hematocrit
Normal MCHC values: 32 – 36% hemoglobin / cell
Calculate your Mean Corpuscular Volume.
o Mean corpuscular volume (MCV) in (um3) = (Hematocrit * 10) / (RBC count)
● Normal MCV values: 76 – 100 um3
o Males: 13 – 18 g/dL
o Females: 12 – 16 g/dL
● Calculate your Mean Corpuscular Hemoglobin Concentration.
o Mean corpuscular hemoglobin concentration (MCHC) in (%) = ( [hemoglobin] * 100% ) / hematocrit
Normal MCHC values: 32 – 36% hemoglobin / cell
Calculate your Mean Corpuscular Volume.
o Mean corpuscular volume (MCV) in (um3) = (Hematocrit * 10) / (RBC count)
● Normal MCV values: 76 – 100 um3
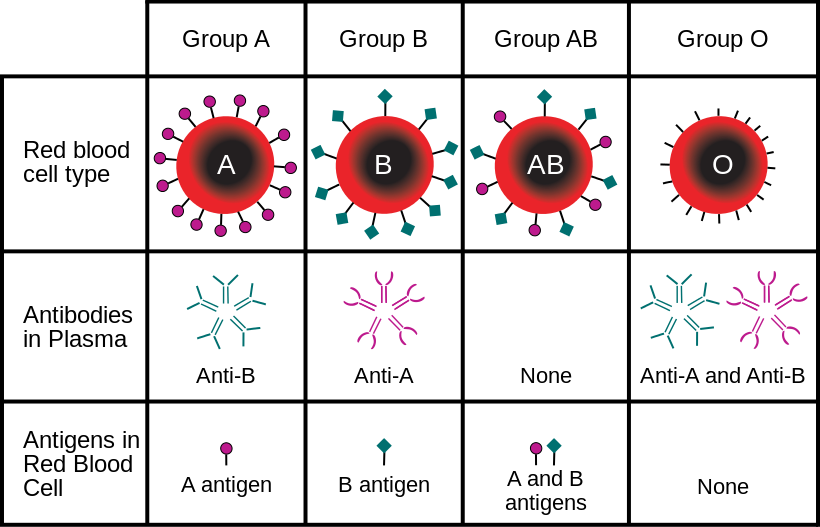
Lab Exercise B. Blood typing
Equipment • Placemat • Lancet • Alcohol swab • Band-Aid • 2 slides • 4 cover slips • ABO blood typing kit (A antibody, B antibody) • Rh blood typing kit (D antibody) • 3 Toothpicks • Wax pencils
Equipment • Placemat • Lancet • Alcohol swab • Band-Aid • 2 slides • 4 cover slips • ABO blood typing kit (A antibody, B antibody) • Rh blood typing kit (D antibody) • 3 Toothpicks • Wax pencils
Protocol:
- 1. Set up your placemat and materials. Read through the entire set of instructions before you begin.
- 2. Use an alcohol swab to clean the area that you will lance. Allow the area to dry.
- 3. Draw two circles on a slide and label A and B. Draw one circle on a slide and label Rh. See the figure for guidance.
- 4. Add one drop of A antibody on the circle labeled A.
- 5. Add one drop of B antibody on the circle labeled B.
- . Add one drop of D antibody on the circle labeled Rh.
- 7. Lance your finger and discard the first drop of blood. Place one drop in each circle on the slides.
- 8. Mix the blood and antibody using a clean toothpick. Use a clean toothpick for each circle/antibody.
- 9. Wait 1 minute.
- 10. Put a coverslip over each circle and look under the microscope.
- 11. Record any hemagglutination. Remember that hemagglutination is considered a positive result.
- 12. CLEAN-UP: Lancets and slides should go in the biohazard sharps waste. Alcohol swabs, used Band-Aids, and any other material that touched blood should go in the biohazard soft waste. Other clean waste should go in the regular trash.
• Blood typing
● Draw your results:
● What blood type are you? __________________________________ ● List the blood types could you accept during a blood transfusion:
● List the blood types could you not accept during a blood transfusion:
● Explain why a universal donor can donate to anyone but can only accept from one blood type.
● Draw your results:
● What blood type are you? __________________________________ ● List the blood types could you accept during a blood transfusion:
● List the blood types could you not accept during a blood transfusion:
● Explain why a universal donor can donate to anyone but can only accept from one blood type.
Blood type |
Type A |
Type B |
Type AB |
Type O |
Antigens Present (on RBCs) |
Type A Antigen |
Type B Antigen |
Type A and Type B Antigens |
No Antigens (Universal Donor) |
Antibodies Present (in blood plasma) |
Type B Antibodies |
Type A Antibodies |
No Antibodies (Universal Recipient) |
Type A and Type B Antibodies |
Exposing RBCs to Anti-A Antibody RESULTS |
Agglutination - Anti A Antibody Binds to the Type A Antigen |
No Agglutination |
Agglutination - Anti A Antibody Binds to the Type A Antigen |
No Agglutination |
Exposing RBCs to Anti-B Antibody RESULTS |
No Agglutination |
Agglutination - Anti B Antibody Binds to the Type B Antigen |
Agglutination - Anti A Antibody Binds to the Type A Antigen |
No Agglutination |
CAN RECEIVE BLOOD TYPES |
Blood Type A and Blood Type O |
Blood Type B and Blood Type O |
Blood Type A, Blood Type B and Blood Type O |
Blood Type O |
Rh Factor |
Rh + |
Rh - |
Antigens Present (on RBCs) |
Rh + Antigen |
No Antigen |
Antibodies Present (in blood plasma) |
No Antibodies |
Rh Antibodies |
Exposing RBCs to Anti-Rh Antibody RESULTS |
Agglutination - Anti Rh Antibody Binds to the Type Rh Antigen |
No Agglutination |
CAN RECEIVE BLOOD TYPES |
Blood Type Rh + and Blood Type Rh - |
Blood Type Rh - |
A patient can receive blood that has the same ABO antigens as theirs, plus O.
Rh+ can receive Rh+ or Rh-, while Rh- must receive Rh- blood.
Rh+ can receive Rh+ or Rh-, while Rh- must receive Rh- blood.
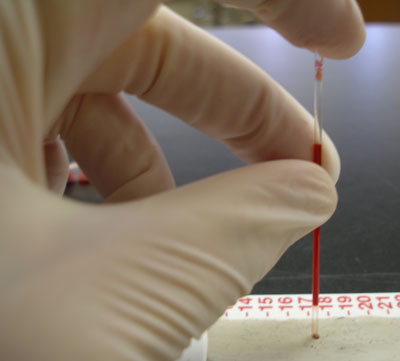
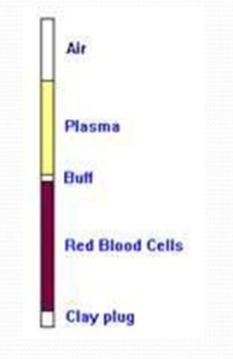
Lab Exercise C. Hematocrit Level
Hematocrit (Hct) Levels. This is the ratio of the volume of red cells to the volume of whole blood. Normal range for hematocrit is different between the sexes and is approximately 45% to 52% for men and 37% to 48% for women.
|
Equipment • Placemat • Hematocrit tube (Heparinized capillary tube) • Clay sealant • Hematocrit centrifuge • Hematocrit reader Protocol:
|
When heparinized blood (heparin is an anticoagulant) is centrifuged, the red blood cells become packed at the bottom of the tube, while the plasma is left at the top as a clear liquid. The ratio of the volume of packed red cells to the total blood volume is called the hematocrit.
|
● What is the purpose of using a hematocrit centrifuge?
|
Centrifuges apply centrifugal force to separate suspended particles from a liquid or to separate liquids of different densities. These liquids can include body fluids (e.g., blood, serum, urine), commercial reagents, or combinations of the two with other additives. By creating forces many times greater than gravity, centrifuges can greatly accelerate separations that occur naturally as a result of density differences. The microhematocrit centrifuge, a special-purpose version of a fixed-head unit, quickly attains speeds of 11,000 rpm and RCFs (relative centrifugal forces) of up to 15,000 g to spin microcapillary tube samples. These tubes require only small blood samples taken from a puncture site or from an anticoagulated venous blood specimen.
|
|
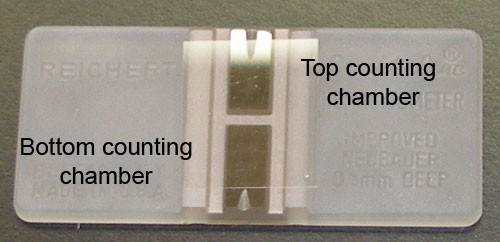
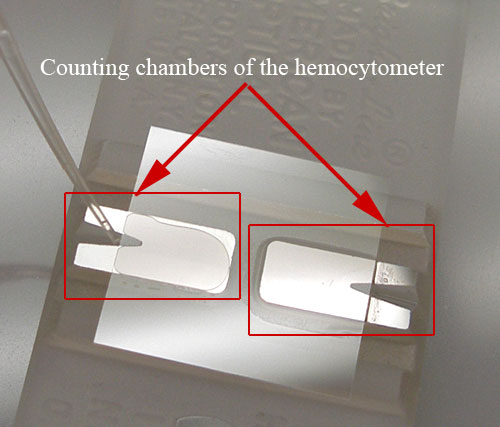
Lab Exercise D. RBC (erythrocyte) Count
***Student will only get to try this experiment one time. Equipment • Placemat • Lancet • Band-Aid • Alcohol swab • Hemocytometer • Unopette reservoirs (small microcentrifuge tube with fluid) • Small capillary tube for unopette reservoir • Counter • Micropipette Protocol:
|
Counting
Observe the grid of the hemocytometer. Different areas are used for counting red blood cells and white blood cells. You will count the red cells that are located in the areas indicated in red. Consider the following: The central grid of 25 squares is 1mm x 1mm in area and 0.10 mm deep, and holds 0.1ml of liquid. The dilution factor is 1:200. Convert the number of red blood cells that are counted in 5 squares to the number of red blood cells/µl. (N.B. 1 µl (microliter) = 1 cubic mm ). Since only 5 out of the 25 squares (1:5) are counted, you must multiply your count by 5. Since you have diluted your sample by 200 (1:200), you must also multiply your count by 200 to arrive at the original concentration in the body. You obtain a count which is contained in a volume of 0.1µl (25 squares). So you must also multiply by 10 to express the count per cubic mm. Important note: To avoid counting the same cells twice, cells that are touching the lines at the tops and left sides of the squares are counted, but cells that are touching the bottoms and right sides of the squares are not counted. Typical Counts for Female: 3.9 to 5.6 million/µl Typical Counts for Male: 4.5 to 6.5 million/µl RBC count for Square 1: ___________________________________ ● RBC count for Square 2: ___________________________________ ● RBC count for Square 3: ___________________________________ ● RBC count for Square 4: ___________________________________ ● RBC count for Square 5: ___________________________________ ● Total RBC count for Squares 1-5: ____________________________ ● Multiply the above number by 10,000: _________________________ ● Normal RBC counts vary for males and females:
o Males: 4,200, 000 – 6,900,000 μL/mm3 o Females: 3,900, 000 – 5,600,000 μL/mm3 ● Are you within normal range? _______________________________ |
Excessively low values of red blood cell count, hematocrit, or hemoglobin may be indicative of anemia (i.e. decreased oxygen carrying capacity of blood). There are many different causes of anemia (e.g. loss of blood through hemorrhage, bone marrow disease, iron deficiency, vitamin B12 deficiency, or folic acid deficiency, etc.) and some of those are characterized by typically very small or very large red blood cells or reduced hemoglobin concentration in each cell.
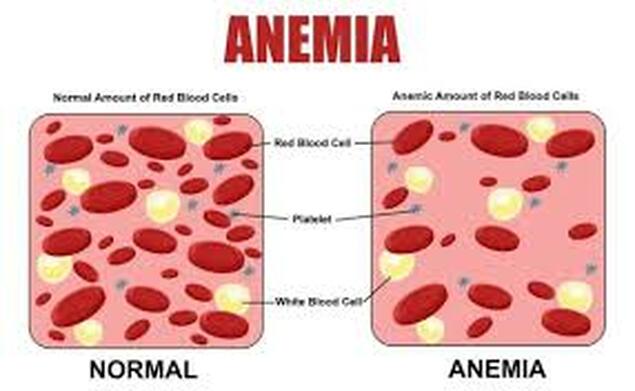
Diagnosis of the type of anemia may be assisted by relating the measurements of red blood cell count, hematocrit and hemoglobin to derive the mean corpuscular volume (MCV) and the mean corpuscular hemoglobin concentration (MCHC).
Erythrocytes containing the normal amount of hemoglobin (normal MCHC) are called normochromic. When the MCHC is abnormally low they are called hypochromic, and when the MCHC is abnormally high, hyperchromic.
Erythrocytes containing the normal amount of hemoglobin (normal MCHC) are called normochromic. When the MCHC is abnormally low they are called hypochromic, and when the MCHC is abnormally high, hyperchromic.
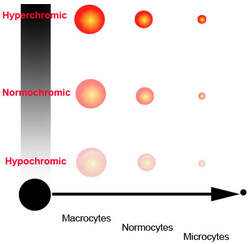
Erythrocytes that have a normal size or volume (normal MCV) are called normocytic. When the MCV is high, they are called macrocytic. When the MCV is low, they are termed microcytic.